The first time I told someone I had Crohn's disease outside of my close group of friends who originally knew about my diagnosis was just a couple weeks after Kevin and I started dating. We were standing outside his car in the Downtown Disney parking lot, and it was 2pm. My phone alarm went off to remind me to take my medication. I didn't have any water with me (as usual), so I popped two bright blue horse pills in my mouth and swallowed them dry. Kevin had seen this a couple of times, but on this particular occasion, asked what I was taking and why. I told him I have Crohn's disease, and had to take these pills 3 times per day. His reaction? "Crohn's disease? Like Kurt Cobain?"
Having a chronic illness means I've taken a lot of medications over the past 10 years, some more innocuous, and some more intense. I've been on everything from steroids to chemotherapy drugs to antibiotics to biologics, and it seems like everything in between. Below is an exciting tale of my drug cocktail (and costs) over time!
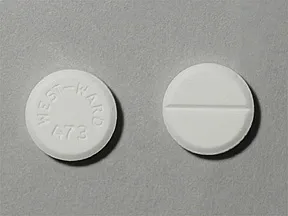
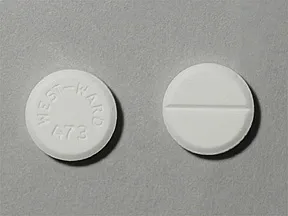
Prednisone (steroid)
Total Cost: $154 / 30 days
Cost with insurance: $154 / 30 days
 |
| Prednisone |
The first medication I was prescribed was a steroid, Prednisone, to help reduce the inflammation in my small intestine. Prednisone is probably my least favorite med I have taken for Crohn's, not because the meds themselves were awful, but rather because of the side effects. First, I had "moon face," or swelling in the face (and other body parts) from water retention. This is a common side effect of Prednisone. The other side effect was the crazy mood swings. I don't remember specifics, but I do remember feeling crazy and having no control over my emotions or reactions, which for a 20-year old girl about to travel abroad for a semester, was not a fun time. The longer-term effects of these pills is osteoperosis. I had to take Prednisone for 20 weeks, starting at 20mg for 4 weeks, then dropping down the dose by 2mg every week until I reached 0, which was almost the entire time I was living in Salzburg.
Pentasa (mesalamine)
Total cost: $3,257 / 30 days
Cost with insurance: $70 / 30 days
 |
| Pentasa |
The other medication I took when I was first diagnosed was Pentasa. I was prescribed two bright blue pills, three times per day. From 2008 until 2012, I took those pills with me everywhere I went to take at 8am, 2pm, and 8pm. I had to set an alarm on my phone to remind myself that it was drug time, though about 50% of the time, I didn't have water with me when it was time to take them, so I dry-swallowed 2 big blue pills on the regular, and got pretty good at it. About a week prior to my hospitalization in 2011, my doctor increased my frequency of these lovely pills to 4 times per day (8 pills each day!)
Bifera (ferrous sulfate)
Total cost: $137 / 30 days
Cost with insurance: $70 / 30 days
 |
| Bifera |
I've always had slightly low iron counts, and have been on and off iron pills since I was a teenager. My iron levels kept getting lower and lower - I was sometimes so anemic that I was ineligible to swim in college and had to do a lot of work to get my iron levels back up. Regular iron pills didn't always work for me, so my doctors would prescribe Bifera, a prescription-strength iron supplement.
Entocort (budesonide; steroid)
Total cost: $1,795 / 30 days
Cost with insurance: $15 / 30 days
 |
| Entocort |
My first minor flare after my diagnosis happened around 2010. Instead of hopping off to the hospital, my doctor wanted to try a steroid, but not Prednisone, since it is so nasty. These little guys are specially formulated to dissolve as they pass through the small intestine, so they release the medication right where it is needed for Crohn's disease. Of course, doctors always prescribe 3 pills per day (all at once) for maximum effect.
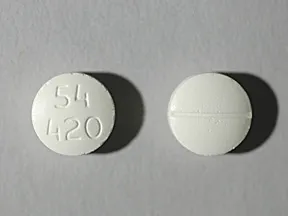
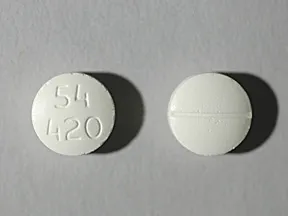
Mercaptopurine (6-MP)
Total cost: $98 / 30 days
Cost with insurance: $0 / 30 days
 |
| Mercaptopurine |
Next came the more intense drugs. After my first hospitalization in 2011, my doctor first added in Mercaptopurine, or 6-MP, a chemotherapy drug also commonly used to treat Inflammatory Bowel Disease (Crohn's or Ulcerative Colitis). The scary possible side-effects of this medication luckily haven't affected me to this point. I'm still taking it to this day, though on double the dose I started on in 2011 (it was doubled after my second hospitalization in 2013). The one side effect I have really experienced has only been observed in my routine blood work, with some slightly elevated liver levels, though nothing to be too worried about (yet).
Ferric Gluconate (IV iron supplement)
Total cost: $340 / infusion
Cost with insurance: $0 / infusion
 |
| Sodium Ferric Gluconate |
In 2011, not long after I stared grad school in San Diego, my iron levels were significantly lower than normal (me: 8.7; normal: 11-14; below 9 is critical - no wonder I was so tired!) I started seeing a Hematologist at Sharp HealthCare (Dr. Andrew Hampshire), who prescribed me an iron infusion, since my iron pills clearly weren't working, but we didn't want to go too extreme with a blood transfusion, unless it was necessary. In 2011, I received three iron infusions over the course of three weeks; then in 2012, I received two additional infusions over two weeks when my iron levels were too low again.
Humira (adalimumab; biologic)
Total cost: $2,523 / 28 days
Cost with insurance: $0 / 28 days (with prior authorization)
 |
| Humira |
In 2012 after a test showing my small intestine had formed a fistula, my doctor wanted to increase the intensity of the medications, and recommended I start a biologic medication. These are the ones you see advertised all the time on TV comercials: Humira, Stelara, etc. He gave me the choice between Humira and Remicade to start. Humira meant I could still take the medications at home on my own, but would have to give myself a shot every two weeks. Remicade, on the other hand, was only every 8 weeks, but I would have to go in to a medical office for a 3+ hour IV. At that time, I elected to go with Humira. Kevin really enjoyed giving me those shots every other Saturday, so I let him do that when he was home, because I hated it. I would rotate my shots from right leg to left leg to left stomach to right stomach, then start that rotation again. After my surgery in 2013, my doctor decided to keep me on Humira; she felt that the reason I had not reacted as well was because my disease was too far progressed. With the major issues removed by surgery, I was able to stay on Humira in remission for almost two more years.
Remicade (infusion; biologic)
Total cost: ~$18,000 / 8 weeks
Cost with insurance: ~$1,500 / 8 weeks (with prior authorization)
 |
| Remicade (IV) |
Once it was clear that the Humira wasn't working anymore, my doctor originally prescribed me Entivyo, but my insurance company denied the prior authorization, saying that they wanted me to try Remicade first. So here we are. Every 8 weeks, I receive an infusion of Remicade, a 3+ hour procedure, which typically takes place in an infusion center, but since moving to Las Vegas, I have been lucky enough to get a home infusion - a nurse comes to my house, sets me up, mixes the meds, and hangs out with me for 3 hours. The most frustrating part of this whole process has been the prior authorization process. Everyone (doctors, insurance company) has been really slow about getting everything approved, something that has to happen once per year AND every time I move (which has happened a lot in the past 16 months...)
Biologics, Mercaptopurine, and steroids all decrease the immune system, so the main side effect I have from all of these medications is secondary infections... most recently including Shingles, because instead of 30, my body thinks its 75. This drug cocktail serves as a strong reminder that there is no cure for Crohn's disease. All of these medications are designed to keep the disease at bay, but can loose their effectiveness without warning.
Let's find a cure for Crohn's!
This year, I am once again taking part in Team Challenge, participating in the Lake Tahoe Triathlon at the end of August for my 10 year anniversary of being diagnosed. You can support my fundraising efforts
here.
----
Stay tuned for Part 4:
Doctors